How Can You Treat Peripheral Arterial Disease?
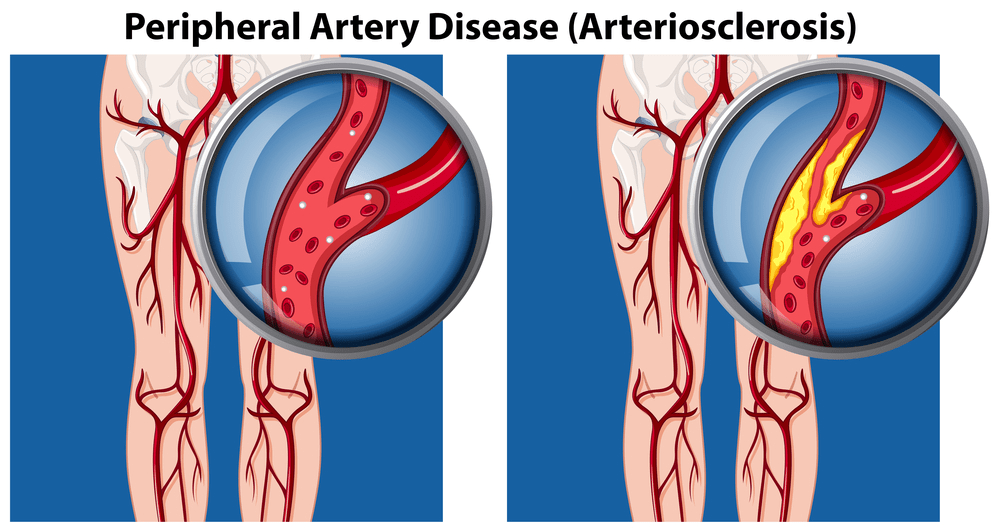
Every year, 6.5 million Americans aged 40 and over suffer from peripheral arterial disease, or PAD. This common circulatory problem is characterized by painful cramping, numbness, weakness, and coldness. Today, our vascular experts at Zenith Vascular & Fibroid Center in Memphis, TN are discussing everything you need to know about this disease, including how it is treated. Here’s what you need to know.
How Can You Treat Peripheral Arterial Disease?
While there is no cure for PAD, the symptoms of this disease can be managed with treatment. Treatment can also mitigate your risk of stroke or heart disease. Treatment techniques for this condition are unique to the individual suffering from the disease because everyone’s symptoms are different and people are in different stages of the disease. Some of the most common treatment methods used are:
- Taking blood pressure medication
- Smoking cessation
- Taking blood-thinning drugs
- Managing bad and overall cholesterol levels
- Managing blood sugar levels
Note, one of the best things you can do for the treatment of PAD is to maintain a nutritious diet and manage symptoms with exercise. No more than 30% of your daily calories should come from fat, and no more than 7% of your daily calories should come from saturated fat. In other words, you should keep your fat consumption to a minimum and keep your saturated fat consumption to a bare minimum. Focus on eating reasonable portions of monounsaturated and polyunsaturated fats.
Other Diet and Lifestyle Tips to Improve Your PAD Symptoms
If possible, you should not consume products containing trans fats. This includes foods and beverages that contain hydrogenated and partially-hydrogenated vegetable oils. You can also improve your PAD symptoms by reducing your sodium intake and taking blood pressure medication or increasing your potassium intake to counteract the sodium in your diet.
You may also benefit significantly from choosing foods that are high in soluble fiber and low in cholesterol. Finally, you should make a point to walk regularly. Walking may not be comfortable at first, but the more you walk, the easier walking will become for you.
Do I Have PAD?
To determine whether you suffer from peripheral vascular disease, you need to come in for an initial consultation. There are several ways this condition can be diagnosed, but the most commonly used diagnostic tool is the ankle-brachial index. During this examination, we will compare the blood pressure in your arm and ankle. This is accomplished using a standard blood pressure cuff and an ultrasound device that shows the flow and pressure of your circulating blood.
However, an ankle-brachial index is not the only diagnostic tool we have in our toolbox. We can also diagnose peripheral vascular disease through a physical exam. During your physical exam, we will look for such signs of PAD as whooshing sounds over your arterial passageways, hypotension, slow wound healing, or an extremely weak pulse.
What Are the Most Common Symptoms of PAD?
Many people who have this condition experience mild or no symptoms. Occasionally, claudication is present. Claudication is a condition characterized by painful muscle cramping in your extremities that is triggered by activity but subsides after a period of rest. Learn more about claudication at ZenithVascular.com For example, your calves may start to burn after walking or your forearms may painfully cramp while cooking dinner.
Eventually, claudication may worsen to the point you can’t even sleep and any reprieve is hard-earned and temporary. For instance, you may wake up in the middle of the night due to intense muscle cramping and only earn a brief respite after pacing around your room slowly for several minutes. Other symptoms of peripheral arterial disease include:
- Coldness in the affected area
- Leg hair loss
- Ulcers
- Thinning skin
What Risk Factors Are Associated With This Disease?
According to the American Heart Association, there are a number of factors that increase your risk of developing peripheral arterial disease. For example, the likelihood that you develop PAD increases if you:
- Consume tobacco products
- Have hypertension
- Have high cholesterol
- Have diabetes
- Are age 60 or older
- Have a BMI over 29.9
- Have a family history of vascular conditions
- Have renal failure
Here’s a closer look at some of the risk factors for developing this disease:
Having Hypertension
Having hypertension (high blood pressure) is one of the most significant risk factors for developing PAD. Remember, this disease cannot be cured; it can only be treated. Therefore, if you have PAD and high blood pressure, it is of the utmost importance to manage your blood pressure moving forward.
This is because PAD increases your risk of having heart disease or a stroke, and high blood pressure alone also increases these risks. If you have both PAD and high blood pressure, your risk of heart or brain problems increases significantly.
Consuming Tobacco Products
It doesn’t matter whether you currently consume tobacco products or only have a history of consuming tobacco products. If you are a smoker, used to be a smoker, or have ever consumed nicotine in any other form, you are at an increased risk of developing peripheral vascular disease. Consuming tobacco products puts you at a significantly increased risk of developing PAD because the chemicals in tobacco products cause severe inflammation.
In addition to causing severe inflammation, the chemicals present in tobacco products accelerate the rate at which arterial plaque builds up. In other words, it can cause atherosclerosis, a dangerous condition that can lead to peripheral vascular disease.
Being Over 59 Years Old
Age is another very significant risk factor for developing peripheral vascular disease. The older you are, the more time has passed to allow plaque to build up in your arteries.
Do I Need to See a Vascular Specialist?
You should see a vascular specialist if you are experiencing serious symptoms that may indicate the presence of this disease, such as numbness or painful cramping triggered by activity. Additionally, you may want to schedule a screening if you are:
- 66 or older
- 51 or older and diabetic or a smoker
- 50 or younger with multiple risk factors
What If I Don’t Seek Treatment?
Often, the worst that happens to people who don’t seek treatment for this condition is worsening symptoms. However, complications may arise if you do not seek treatment for this condition. For example, people who do not seek treatment for peripheral arterial disease may develop a condition known as critical limb ischemia.
This condition first presents itself as non-healing open sores, infections, or injuries on the legs or feet. Eventually, tissue death can occur to the point that limb amputation is necessary. Additionally, other vascular conditions may develop because atherosclerosis can develop anywhere. For instance, arterial fatty deposits may impede circulation to your heart or brain. This may lead to heart disease or a stroke.
Amputation
If you are diagnosed with peripheral arterial disease and you have diabetes, it is of the utmost importance that you keep your diabetes well-managed. Sometimes, people with diabetes need to have a foot amputated due to extremely slow-healing wounds. However, if you have both uncontrolled diabetes and PAD, your risk of needing a partial or total foot or leg amputation is much greater. This is because PAD also slows down wound healing.
How Should I Prepare for My Appointment?
The most important thing you should do to prepare for your appointment is to stop smoking and consuming other tobacco products. Whether you suffer from PAD or not, nicotine consumption is a significant risk factor for the development of PAD and other vascular disorders. You can also prepare for your appointment by:
- Taking copious notes of your symptoms
- Losing weight
- Eating nutritiously
- Exercising regularly
Learn more about smoking and PAD risk factors.
Schedule Your Initial Consultation Today
Neither leg pain nor numbness are normal parts of the aging process. If you are experiencing either of these symptoms, you may have PAD. This disease cannot be cured, but it can be treated with lifestyle changes and medications that will help you manage your symptoms and reduce your chance of having a stroke or heart disease. Contact us today at Zenith Vascular & Fibroid Center in Memphis, TN to schedule an appointment and learn more.






